Table of Contents
Coronavirus causes Thrombosis
COVID-19 increases the risk of blood clots (thrombosis) in the heart, lungs, blood vessels and other organs.
Blood clots can cause strokes, heart attacks and multiple organ failure, eventually leading to death.
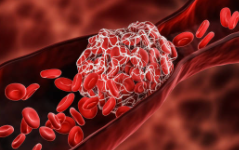
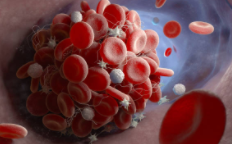
A thrombosis is a kind of accumulation of “glued” platelets, which is formed as a result of increased blood clotting.
A blood clot, in general, is such a cast of blood cells and blood proteins, it is such a two-component ball. Blood clots can constantly form, break down, they can be arterial and venous…
Why does coronavirus cause thrombosis?
Scientists have identified three potential causes of this problem at once:
1. Damage to the inner wall of blood vessels
Even with minor injuries, the blood becomes thicker to prevent severe blood loss.
That is, this mechanism should be useful. However, with a large number of blood clots, blood circulation is impaired, and dangerous complications can develop.
2. Stagnation of blood during hospitalization
Blood circulation in the veins is largely dependent on muscle contraction. When people walk or run, muscles constrict blood vessels and help push blood to the heart.
In the hospital, patients move little. Because of this, blood more often accumulates in the veins and blood clots often form in it.
3. Increased blood clotting
When infected with coronavirus, a special protein is activated in the body, which affects the functioning of the immune system.
As a result, the blood becomes thicker and the risk of thrombosis increases.
Among the causes of thrombosis in coronavirus, doctors consider the third factor the most important – the body’s response to a viral attack.
So let’s take a closer look at it.
A whole system of proteins circulates in the blood. They identify and neutralize viruses, bacteria and damaged cells.
Under normal conditions, these proteins cleanse the body of dangerous elements without harming the body itself.
However, with coronavirus, the defense system is too active and damages tissue, which increases the likelihood of thrombosis.

The first Signs of thrombosis in coronavirus
Not all patients have symptoms of this disease. Therefore, the absence of symptoms of thrombosis after coronavirus does not guarantee protection against pulmonary embolism.
Under normal circumstances, this complication is rare. However, with a severe form of COVID-19, the likelihood of blood clots increases more than tenfold. So blood clots are more likely to end up in the lungs.
How does deep vein thrombosis manifest after coronavirus?
Patients with this disease are often diagnosed with the following symptoms:
- Edema
In most cases, stagnation of lymphatic fluid occurs in only one limb. Sometimes the swelling affects both legs. - Pain
Unpleasant sensations often arise in the calves, and then spread to the limb. More pain appears during seizures. - Pallor of the skin
In the affected area, blood circulation is impaired. The skin does not receive enough oxygen and gradually takes on a painful appearance. - Redness and warmth in the leg. These signs usually indicate inflammation of the venous walls.
If blood clots form in superficial vessels, then the pathology manifests itself more clearly and more strongly affects the patient’s quality of life
How to prevent Thrombosis?
Taking aspirin can reduce the risk of death from COVID-19, American scientists have found. By thinning the blood, it prevents blood clots(thrombosis) from forming, thereby reducing the risk of stroke and other organ damages.
If these results can be confirmed, aspirin could become a cheap and massive coronavirus prophylaxis.
Researchers followed 412 patients hospitalized with COVID-19. About a quarter of them took low-dose aspirin (about 80 mg) for the week before hospitalization.
It turned out that in such patients the risk of being in the intensive care unit was reduced by 43%, the need for mechanical ventilation appeared 44% less often, and they also died in the hospital 47% less often.
Patients taking aspirin did not have a significant increase in complications, such as severe bleeding.
The result was the same when other factors, such as age, gender, body mass index, race, presence of hypertension and diabetes, were taken into account.
Also taken into account were diseases of the heart, kidneys, liver and the use of beta-blockers to control blood pressure.
Don’t sit still for more than an hour
Venous circulation depends on the movement of the leg muscles. The longer a person sits or stands motionless, the more often the blood stagnates in the vessels.
Yes, during self-isolation, people are afraid to go for a walk. However, to reduce the risk of thrombosis, it is not necessary to walk on the street for hours near potential sources of the disease.
Even a short walk at home will disperse the blood in your veins. Just get out of your chair or sofa and walk around the apartment for five minutes. Repeat this every hour.
When walking, muscles constrict blood vessels and push stagnant blood to the heart, which reduces pressure on the venous walls and reduces the risk of thrombosis.
Quit smoking
For many, during the pandemic, bad habits only worsened. For example, some people smoke more often to ease feelings of anxiety.
Smoking increases the likelihood of blood clots forming, and therefore this habit will prevent you from avoiding deep vein thrombosis in coronavirus.
Yes, not everyone will be able to immediately give up cigarettes. But any reduction in your daily dose of nicotine will still benefit your vascular health.
Fight excess weight
The blood volume is 7-8% of the body weight.
The increase in weight inevitably leads to increased stress on the venous walls and valves. The more blood in the vessels, the higher the likelihood of stagnation.
That is, in overweight people, blood more often accumulates in the veins, which increases the risk of thrombosis.
Calculate your optimal weight first. For this, two formulas are used: (Height (in cm) – 110) * 1.15) – for men, (Height (in cm) – 100) * 1.15) – for women.
Try not to deviate too much from the norm. However, a difference of a few kilograms will hardly affect the likelihood of blood clots.
THROMBOSIS Final Words
Seeing a doctor is always a must, especially if you know you are at increased risk.
It is very important to know yourself and your family history: if the family had any problems with the veins – at least go to a therapist, discuss whether something needs to be done or not
